
In 2014, federal agencies issued draft recommendations that women who are pregnant, breastfeeding or might become pregnant and young children eat more fish that is lower in mercury. Their advice is based on the fact that seafood consumption is an excellent source of omega-3 fatty acids and other nutrients.
EWG felt the advice didn’t go far enough. It would be ineffective, even dangerous, for women who ate too much mercury or fish species low in omega-3 fatty acids.
Now our concerns have been confirmed by a new study.
We enrolled 254 women who eat at least two meals of seafood, fish or shellfish every week and measured the amount of mercury in their hair to assess how much mercury was in their bodies.
We found that almost 30 percent of our participants had too much mercury exposure according to Environmental Protection Agency guidelines for pregnant women. Much of their exposure was tied to fish species like tuna steaks and sushi that are not included in the government’s warning.
What You Can Do
1. Watch Our Video
EWG’s 2-minute video is the best way to hear about the findings and recommendations from our study.
2. Read the report
If the video made you want to learn more, you can read the full report here.
3. Educate Yourself
 EWG provides guidelines for choosing seafood high in omega-3 fatty acids and low in mercury. Here’s how to check them out.
EWG provides guidelines for choosing seafood high in omega-3 fatty acids and low in mercury. Here’s how to check them out.
- Calculator: Use our calculator to get a custom seafood list – based on your age weight and more.
- Guidelines: We also have general guidelines that fill the gaps of the federal government’s flawed guidance.
- FAQs: Still have questions about seafood, mercury or omega-3 fats? Check out our frequently asked questions.
4. Tell Your Friends
Let your friends know who would be interested in protecting themselves against too much mercury exposure.
Executive Summary
 To protect your baby from toxic mercury and ensure his or her healthy development, you should not only watch how much fish you eat, but what kind of fish.
To protect your baby from toxic mercury and ensure his or her healthy development, you should not only watch how much fish you eat, but what kind of fish.
Federal agencies advise women who are pregnant, nursing or planning to become pregnant to eat much more seafood, an excellent source of the omega-3 fatty acids essential to babies’ development. The most recent draft recommendations from the Food and Drug Administration and the Environmental Protection Agency say these women should eat eight to 12 ounces of fish and shellfish a week – more than twice as much as the average American.
The agencies also list fish they say are lower in mercury, a powerful neurotoxin harmful to the developing brains of fetuses, babies and young children. The aim is to encourage seafood consumption without overdoing the mercury. Among almost all experts, in recent years this goal has supplanted the once-prevailing view that to avoid mercury pregnant women should eat less fish or even cut it out of their diet altogether.
“When you eat seafood during pregnancy, you get the benefits from omega-3s but from mercury you have the risk of toxicity,” said Dr. Philippe Grandjean, an adjunct professor at the Harvard School of Public Health. “If you get a little bit of mercury it can be offset by the omega-3s. But that means you don't get the full benefit of the omega-3s and other nutrients in seafood. So women should minimize mercury exposure because only then will they get the maximum benefit of seafood.”
Now a new EWG study finds that adhering to the federal government’s recommendations on seafood and mercury may be risky, potentially leading women to eat too much of the wrong kind of fish. Nationwide testing found that mothers who eat the species of fish in the amounts recommended by FDA and EPA risk exposing their babies to harmful doses of mercury while not providing them with enough healthy omega-3s.
EWG recruited 254 women of childbearing age from 40 states who reported eating as much or slightly more fish than the government recommends. A university lab tested samples of their hair, where mercury accumulates and reflects the level in the body as the hair grew.
Nearly three in 10 of the women had more mercury in their bodies than the EPA says is safe – a level many experts say is much too high for pregnant women. Almost 60 percent of participants had more mercury than a stricter limit recommended by Grandjean, who analyzed hair samples for EWG’s study, and scientists from two prestigious European institutions. The frequent seafood eaters had an average of 11 times as much mercury as a comparison group who eat seafood rarely, proving that the high mercury levels came from the fish rather than other sources.
Mercury emissions from coal-fired power plants and other industrial sources are carried by air and deposited on oceans and waterways. Bacteria convert it to methylmercury, the form that accumulates in fish and is most harmful to human health. In the U.S., an estimated 75,000 infants born each year are exposed in the womb to potentially harmful levels of mercury.
To limit mercury consumption, FDA and EPA recommend that women eat no more than six ounces a week of canned albacore tuna and no shark, swordfish, tilefish or king mackerel. But our study suggests that many women who follow that advice will not have low enough levels of mercury or get enough omega-3s in their diets.
Our analysis of the women's dietary surveys found that while only a small amount of their mercury intake came from species the government says to avoid or limit, the great majority of the toxin came from species the government does not warn against, especially tuna steaks and tuna sushi. And although the women in our study eat more than twice as much fish as the average American, almost 60 percent still don’t get the amount of omega-3s recommended during pregnancy from seafood in their diets.
In light of the tradeoff between mercury and omega-3s, and because seafood harbors other contaminants, some people believe it is safer to avoid fish completely during pregnancy. We don’t agree.
Researchers overwhelmingly recommend low mercury fish as the most reliable source of omega-3s.The mercury in seafood erodes the benefits of an otherwise healthy food, and in some cases tips the scale to the point that the fish becomes harmful. The tradeoff is like exercising outdoors even when the air quality is less than ideal: Air pollution erodes the benefits of outdoor exercise, but in most cases it is still worth it. If air quality is bad enough, you should stay indoors.
EWG and the Mercury Policy Project urge FDA and EPA to update their recommendations to specify the full list of low mercury-high omega-3 fish, such as salmon, that women should add to their diets. This information is already included in the most recent edition of the Dietary Guidelines from the Department of Agriculture and the Department of Health and Human Services, so aligning the recommendations would provide greater clarity to the government’s advice, which doctors and other health professionals look to for guidance.
The advice should also educate women about the hazards of mercury and name additional species they should limit or avoid for up to a year before conception, such as seabass, halibut and marlin.
In the absence of government action, EWG’s Good Seafood Guide provides model guidelines for consumers looking to reduce intake of mercury consumption and increase intake of omega-3 fats. The EWG Seafood Calculator estimates portion size and frequency based on a child or adult’s weight and recommends that pregnant women and children ingest 25 percent less mercury than the current EPA guideline.
Findings
Since 2010 federal agencies have recommended that all adults eat eight to 12 ounces of fish and shellfish per week. In 2014 the FDA and EPA issued a draft recommendation that pregnant women eat the same amount.1 Currently, the average American adult eats 3.5 ounces of seafood a week.2
The recommendation to eat more seafood during pregnancy is primarily based on the benefits of two long chain omega-3 polyunsaturated fatty acids in fish and shellfish, referred to as DHA+EPA (docosahexaenoic acid and eicosapentaenoic acid). A diet rich in these omega-3s during pregnancy has been shown to boost babies’ brain development and improve their vision.3 Seafood is also a good source of high-quality protein and vitamins B and D, iodine and selenium.
The amounts of omega-3s and mercury in seafood vary widely depending on species. Women who increase the amount of fish in their diets without choosing the right species may not only fail to get the omega-3s they need but also risk ingesting too much mercury.
To investigate the implications of the federal seafood recommendations for pregnant women, we recruited online almost 300 women of childbearing age. We asked them to fill out a detailed questionnaire about the seafood they ate recently. From this information we chose 254 women in 40 states who ate as much as or slightly more than the FDA and EPA recommend. For comparison, we chose another 29 women who ate seafood rarely or not at all.
We collaborated with the University of Southern Denmark to measure the concentration of mercury in samples of the participants’ hair. The lab analyzed a small strand of hair taken closest to the scalp (two centimeters, about three-fourths of an inch) which reflects mercury ingested in the previous one to three months.
The hair of almost 30 percent of the women who reported eating seafood often had more mercury than EPA’s outdated exposure guideline of one part per million, a level that has now been associated with clear risks to a developing fetus. Nearly 60 percent of the women exceeded 0.58 part per million, the level Grandjean and other researchers say is a more protective upper limit for pregnant women.4 (A part per million is equal to one drop of water in 50 liters, or about 13 gallons, underscoring how tiny amounts of mercury are harmful.)
Mercury levels in the 254 women who frequently eat fish were six times higher than the median level found in a representative sample of all American women in 2004 by the National Health and Nutrition Examination Survey of the Centers for Disease Control and Prevention.5 They had an average of 11 times more mercury than the 29 women who eat seafood rarely, clearly indicating that the high mercury levels came from the fish rather than other sources.
Too many study participants have high mercury or low omega-3s
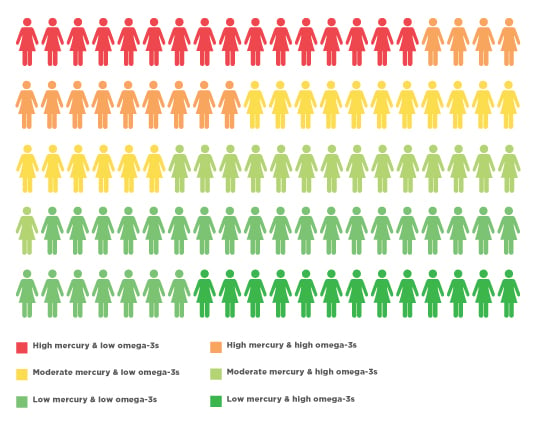
Source: EWG , from 2015 survey and tests of 254 U.S. women of childbearing age
Women with hair mercury levels +/- 1 ppm and estimated omega-3 intake +/- 250 mg of DHA+EPA per day.
Mercury levels in participants’ hair ranged from well below the EPA exposure guideline to 8.8 parts per million – almost nine times as high as the exposure guideline. Mercury levels were greater in those participants who ate higher mercury species frequently, suggesting that the type of fish women eat is more important than how frequently they eat fish and shellfish. (See Methodology Section in report PDF for detailed results.)
The government recommends that adults get an average of 250 milligrams of DHA+EPA daily.6 One study estimates that on average American women of childbearing age get only a third of the recommended amount of omega-3s,7 because most Americans don’t eat much fish and shellfish, and the most popular seafoods are very low in omega-3s.
Even though our study participants eat a lot of seafood, we estimate that six in 10 do not get the recommended amount of omega-3s to support an optimal pregnancy. The median omega-3 our participants got was 230 milligrams per day from seafood alone.
Just over one-fourth of our participants had both enough omega-3 intake and mercury levels below the EPA exposure guideline of 1 part per million. About one in six had higher levels of mercury and lower than optimal omega-3s, a particularly unhealthy combination.
Where do government recommendations fall short?
The 2014 draft recommendations from FDA and EPA advise women who are pregnant, nursing or considering pregnancy to eat eight to 12 ounces of a variety of seafood a week.8 The draft retains the agencies' 2004 recommendations that such women completely avoid four fish high in mercury (swordfish, shark, king mackerel and tilefish), eat no more than six ounces of albacore tuna a week, and eat a maximum of 12 ounces of any other fish or shellfish a week. The draft names several “lower mercury” fish and shellfish, including salmon, canned light tuna, tilapia, cod and catfish. It cautions women and children to limit fish caught from local waterways that may be polluted with mercury or other harmful chemicals.
But our study shows that the government’s advice is not detailed enough.
Participants reported eating lots of tuna steaks and tuna sushi, as well as other fish with high levels of mercury that FDA and EPA don’t mention. Tuna contributed almost 40 percent of the mercury ingested by participants, based on their answers to the questionnaire. Other studies have estimated a similar contribution of tuna to mercury intake in the American diet.9 The inclusion of canned light tuna on the government’s "lower mercury" list is in error, since it is in fact not low in mercury and is a significant source of mercury in women’s diets.
Only About One-Sixth of Participants’ Mercury Intake is From Species the Food & Drug Administration Warns Women to Limit or Avoid During Pregnancy
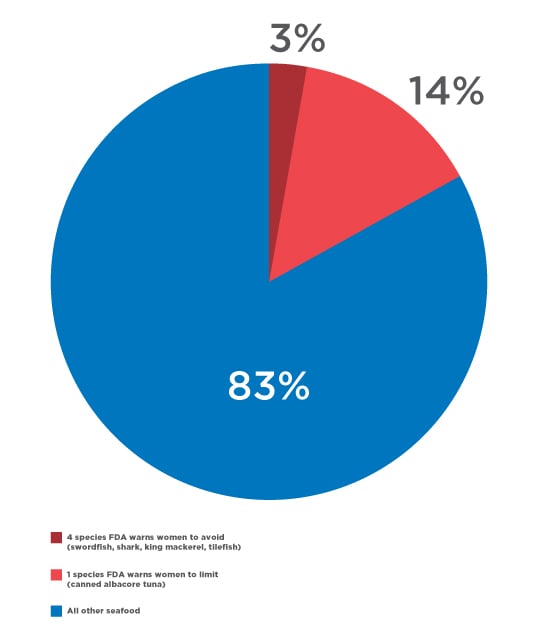
Several other high mercury species contributed an additional 12 percent of participants' mercury intake. These include escolar, walleye and opah – species whose mercury levels are similar to those on the government’s "do not eat" list but are not named in the recommendations – and popular choices like halibut, snapper, seabass, grouper, ono and Spanish mackerel, all with mercury concentrations similar to canned albacore tuna. EWG recommends that pregnant women and children avoid eating these fish whenever possible.
The FDA and EPA recommendations also fail to ensure that women get enough omega-3s. As EWG reported in 2014, eight of the 10 most popular seafood species are too low in omega-3s to be good sources of those fatty acids during pregnancy.10 FDA recommends tilapia and catfish as “lower mercury” species. But a pregnant woman would need to eat about 15 servings of tilapia a week, or 20 servings of catfish, to get the recommended amount of DHA+EPA.
In contrast, wild salmon stands out as a healthy and also popular choice. A single six-ounce serving of salmon can provide an entire week’s worth of omega-3s and is very low in mercury. Our participants eat a lot of salmon and we estimate it provides almost half of the omega-3s in their diets. Small oily fish such anchovies, herring, sardines and shad made up very few of participants' seafood meals but provided almost 15 percent of their omega-3s.
Confusingly, there is another set of federal guidelines for seafood. The recommendations from FDA and EPA are concerned with seafood consumption during pregnancy, while the official Dietary Guidelines of the Department of Health and Human Services and the Department of Agriculture are overarching recommendations about nutrition and health.
The newest Dietary Guidelines, published in January 2016, say all adults (not just pregnant women) should eat eight to 12 ounces of seafood a week. They conclude that people who get an average of 250 milligrams a day of DHA+EPA from seafood have lower risk of dying from heart disease, and consumption during pregnancy leads to improved infant health outcomes.
The Dietary Guidelines provide better detail to help consumers choose fish that are low in mercury and high in omega-3s, listing salmon, anchovies, herring, shad, sardines, Pacific oysters, trout and Atlantic and Pacific mackerel. They advise people to eat these species often to get the benefits of omega-3s.
Many state agencies are also providing their residents with better guidance on seafood safety. For example, California, Connecticut and Washington give clear and practical information about both mercury and omega-3s in commercial fish species.11 FDA and EPA should follow the states’ lead.
What does science say about seafood safety?
In high doses mercury causes serious nerve damage, seizures and birth defects. In the body, mercury creates tissue-damaging free radicals – highly charged, short-lived reactive atoms – and inhibits cellular repairs, making it harmful to the heart, kidney and other body organs. A number of genes appear to affect a person’s ability to metabolize and excrete mercury, and others appear to increase vulnerability to mercury’s toxic effects.12
But of greatest concern for pregnant women, low doses of mercury can provoke subtle and lasting changes to the developing brain and nervous system. There is strong evidence that mercury exposure during pregnancy and childhood causes lifelong deficits in learning, memory and reaction times.
During pregnancy the fetus' brain and nervous system are developing rapidly. Mercury disrupts the normal process by which brain and nerve cells form, connect and organize.
Because the placenta allows mercury from the mother's blood to pass into the fetus, mercury levels in the fetus and umbilical cord blood are consistently higher than in the mother.
Newborns are also highly vulnerable to mercury. However, mercury levels in breast milk are relatively low, and infants and young children are not typically fed a high seafood diet. As a result, public health experts have focused on pre-conception and pregnancy as key times to limit mercury ingestion.
In 2000 the EPA determined that mercury levels in pregnant women's blood should be below 5.8 micrograms per liter of cord blood to ensure that the fetus was not harmed.13 The guideline of 5.8 micrograms per liter in cord blood corresponds to 3.5 micrograms per liter in the mother’s blood14 and roughly one part per million mercury in hair.15
In the 16 years since EPA set its mercury exposure recommendations, new studies have shown that mercury is harmful at lower doses than previously thought. One reason is that harmful effects of mercury in earlier studies were to some degree masked by the benefits of omega-3s and other nutrients in seafood.16 Newer research accounts for this through isolating and independently examining the benefits of omega-3s and the harm of mercury exposure to early childhood cognition, memory and attention.
Most studies find negative effects of mercury exposure in utero, and positive outcomes for children whose mothers eat more high omega-3 seafood or seafood in general. The task is complicated by the fact that each study includes women from different regions of the world, eating different amounts and varieties of seafood that vary in contaminants and beneficial nutrients.
The primary benefits of seafood are thought to come from the omega-3 fatty acids, DHA and EPA. They are a major component of cell membranes in the brain, nerve cells, retina and heart. A diet rich in omega-3s can lower blood triglycerides, and lessens the risk of cardiac disease. Omega-3s also reduce inflammation. Researchers are looking at them to treat diseases like arthritis, macular degeneration of the retina and some mental disorders.
One of the most relevant studies of the effects of seafood consumption for American babies was Project Viva, headed by Dr. Emily Oken of the Harvard Medical School and Harvard Pilgrim Health Care.17 It looked at the relationship between women’s seafood intake and mercury exposure during pregnancy and their children’s intelligence, memory, and motor development at six months and three years.
Oken’s team found a benefit to children whose mothers ate seafood frequently during pregnancy, as long as they kept their mercury levels low. Women who ate more than two seafood meals weekly had kids with better neurological development, while children whose mothers had the highest mercury levels showed subtle neurological deficits.
In Oken’s study, the benefits of eating enough seafood and the harm of ingesting too much mercury during pregnancy were roughly equivalent, with each causing about a 10 percent increase or decrease in children’s memory and visual-motor skills. The research team concluded that children benefit most when mothers eat a substantial amount of seafood, but of species with low mercury. Nearly a dozen studies published since have confirmed and reinforced that conclusion.18
Similar findings were reported in a study with more than 400 women and children from New Bedford, Mass. Women with hair mercury concentrations greater than one part per million when they gave birth had children with increased risk of inattentive and impulsive or hyperactive behavior at age 8. Children whose mothers ate more than two servings of fish a week during pregnancy had a much lower risk of ADHD.19
Another study of children’s visual memory and learning found that every part per million increase of mercury in their mothers’ hair during pregnancy was associated with about a 2.8 point decline in visual memory and 2.2 point decline in verbal memory, after adjusting for estimated omega-3 ingestion.20
However, not all studies report the same effects.
A 2016 study by Jordi Julvez and colleagues, of the ISGlobal Center for Research in Environmental Epidemiology, examined Spanish mothers and children with high seafood-high mercury diets. The study found that greater seafood consumption was generally associated with kids’ better scores on neurodevelopment tests at 14 months and 5 years. The benefits were mixed and declined somewhat for women who ate the most fish. Yet this relationship remained when the authors looked at women who primarily eat higher mercury fatty fish like tuna and swordfish.
However, the researchers noted that this finding doesn’t invalidate previous studies that find mercury to be harmful. Spanish women with higher socioeconomic status tend to eat more seafood, exposing them to more mercury, so other factors could contribute to their kids’ higher scores.21
In 2012 Julvez and his colleagues reviewed results from 27 large epidemiological studies. Many were of people in cultures that eat much more seafood than Americans, but four were of communities with diets comparable with the U.S. The authors concluded that the “majority of the publications describe neurodevelopment impairments, particularly when the exposure was measured during pregnancy.” They also noted that “in some populations, nutrients from fish and seafood seemed to counterbalance the real extent of developmental neurotoxicity due to methylmercury.”22
Phillipe Grandjean of Harvard, described how this balance works:
When you eat seafood during pregnancy, you get the benefits from omega-3s but from mercury you have the risk of toxicity If you get a little bit of mercury it can be offset by the omega-3s. But that means you don't get the full benefit of the omega-3s and other nutrients in seafood. So women should minimize mercury exposure because only then will they get the maximum benefit of seafood.
Numerous researchers have identified fish species that women should limit or avoid due to high mercury or a poor ratio of omega-3s to mercury:
- Gary Ginsberg of the Yale School of Public Health and the Connecticut public health department drew on Oken's work to examine 16 common species. He estimated that nine species would, on balance, harm infants if their mothers ate six ounces a week during pregnancy: shark, swordfish, yellowfin tuna, canned albacore tuna, lobster, sea bass, halibut, cod and canned light tuna.23
- Katrina Smith and Jane Guentzel of Coastal Carolina University identified ahi tuna, sea bass, halibut, snapper, cod and canned mackerel as species with mercury risks that outweigh omega-3 benefits.24
- Kathryn Mahaffey of EPA used data developed by Amy Tsuchiya of the University of Washington to identify additional species – carp, monkfish, sturgeon, marlin, flounder and canned light tuna – as fish too high in mercury with too little omega-3s to be healthy during pregnancy.25
- Marco Zeilmaker and his colleagues at the National Institute for Public Health and the Environment in the Netherlands concluded that for people who eat fish frequently, the negative effects of mercury outweighed the benefits of omega-3s for 70 percent of the species they studied.26 They suggested that women should avoid high mercury fish for up to a year before conceiving.
Clearly the science supports nutritional policies that encourage consumption of high omega-3 seafood. Research that aims to identify and promote consumption of the healthiest species is more scarce.
Emily Oken developed a simple handout to advise women about the amount and species of fish they should eat during pregnancy.27 She found that pregnant women who got the handout raised their level of consumption of the essential omega-3 DHA and kept their level of mercury low. Participants ate even more DHA when they were given a gift card to a grocery store that could be used weekly to buy healthy seafood.
Some researchers and advocates, concerned about contaminants in seafood and the sustainability of fisheries, suggest that people seek out vegetarian sources of omega-3 fatty acids. However DHA and EPA are only found only in fish, shellfish and some algae-derived supplements. Nuts and vegetables, including canola oil, soybean oil, flax seeds, chia seeds and walnuts contain a third type of omega-3 fatty acid known as ALA (alpha-linolenic acid). The body can convert this fatty acid to EPA and then DHA, but in most people only a small part is converted, making these foods a less effective source of the omega-3s essential to a healthy pregnancy.
Who's at risk for mercury exposure?
Between the draft FDA and EPA recommendation for pregnant women, and the Dietary The guidelines from the Departments of Health and Human Services and Agriculture, show federal nutrition advice has clearly shifted toward increased seafood consumption. But the government is ignoring its own research that increasing seafood consumption also increases mercury risks.28 More than a dozen recent studies highlight specific groups at greater risk for mercury exposure.
The Centers for Disease Control and Prevention regularly monitor mercury exposure for the American public. One CDC study found that one-fourth of women eating seafood two or more times per week had mercury concentrations in their blood above 3.5 micrograms per liter – a level that, if they were pregnant, would expose their developing fetus to too much mercury.29
Another analysis of CDC data found the highest levels of mercury in women in coastal regions of the U.S.30, a finding confirmed by studies in Hawaii31, Florida32, Louisiana,33 Alaska34 and New York City.35 Residents of the Great Lakes region also have high mercury levels.36
CDC data also suggests that Americans of Asian, Native American, Pacific Islander or Caribbean ancestry have higher levels of mercury than whites, African Americans and Latinos,37 largely because they eat more fish.38 This finding is affirmed by studies of Japanese Americans and Korean Americans living in Washington state,39 Asian Americans in Chicago and New York City, 40,41 and Native Americans following a subsistence diet in Washington state.42
People who eat fish caught in polluted waterways are also at greater risk for mercury exposure.43 More affluent people are at increased risk,44 perhaps because they eat more expensive fish species, which tend to have more mercury because they are larger and more likely to be high in the food chain. Studies find elevated mercury exposure for people who eat a lot of sushi,45 and other predatory ocean fish like swordfish, marlin, shark or tuna.46
The number and diversity of Americans who are at higher risk of mercury exposure makes it imperative that federal, state, local and tribal health officials help identify women at high risk and provide language- and culture-appropriate messages about seafood safety.
Recommendations
Women who are pregnant, nursing or considering pregnancy should choose fish that are low in mercury and high in omega-3s. EWG’s Good Seafood Guide identifies the safest, most sustainable species. If you don’t eat fish regularly, consider taking an omega-3 supplement while you are pregnant and nursing. If you eat more than 12 ounces of seafood per week, it is even more important to select lower mercury species.
FDA and EPA must improve their draft seafood advice to women. American women and parents of young children urgently need better advice about seafood choices. The FDA and EPA’s seafood advice for pregnant women should follow the lead of the Dietary Guidelines and clearly identify high-omega-3, low-mercury seafood choices. It must also list additional moderate- and high-mercury fish women should limit or avoid for up to a year prior to conception.
Federal agencies must do more to promote seafood safety. Good advice is only a first step toward healthier seafood consumption. It will also take a coordinated effort between federal agencies, health care providers and nutritionists to educate people about healthy fish choices during pregnancy and childhood. A substantial body of research identifies communities at higher risk for mercury ingestion, and should be used to target people at high risk.
Retailers should inform consumers about high mercury fish. Grocery stores, fish markets and restaurants must also play a role in ensuring that seafood consumption provides a net health benefit. Responsible retailers should stop selling very high mercury fish species, and should use warning labels, shelf talkers or posters at the point of sale to highlight moderate mercury species to limit and avoid during pregnancy and childhood.
State and federal officials must continue to reduce mercury emissions into the environment. In the U.S., coal-fired power plants are the largest source of mercury emissions. Gold mining and other historic industrial activities have polluted lakes and waterways where people fish. Despite national efforts to reduce mercury emissions, concentrations of mercury in the marine food chain are rising due to increases in global mercury pollution
The U.S. must comprehensively implement the Minamata Treaty to address global mercury contamination. In 2013 the U.S. joined 127 nations and signed the Minamata Convention, a global treaty committing international governments to reducing mercury emissions, and became the first country to ratify the convention. The treaty is a good start, but mercury contamination will be long lasting. Mercury levels in the global environment are projected to double by 2050 if the Convention is not effectively implemented. This increase in global mercury pollution could lead to greater concentrations in larger predatory fish and increase risk for seafood consumers, as is already being observed in Pacific tuna.




