
Introduction
More than 1,400 chemicals and chemical groups are known or likely carcinogens. Through industrial applications, consumer products and food, water and air, Americans are exposed daily to these cancer-causing compounds, which invade the body and build up in blood and urine.
Federal health officials have measured many of these chemicals in our systems but the scope and range of carcinogenic pollution in people, known as body burden, has not been tallied – until now.
Through a review of the scientific literature and publicly available human biomarker datasets, EWG compiled the first comprehensive inventory of known or likely carcinogens that have been measured in people. We found that up to 420 known or likely carcinogens have been measured in a diverse array of populations.
Exposures to these carcinogens are by no means limited to on-the-job contact with industrial chemicals. Data from the nationally representative National Health and Nutrition Survey, or NHANES, conducted annually by the Centers for Disease Control and Prevention, confirms that many of these carcinogens are in the bodies of Americans not at risk of occupational exposure – indeed, at any given time some people may harbor dozens or hundreds of cancer-causing chemicals. This troubling truth underscores the need for greater awareness of our everyday exposure to chemicals and how to avoid them – and beyond individual choices, the need for stronger, more effective laws and regulations.
Carcinogens detected in biomonitoring studies come from diverse sources, including:
- Industrial chemicals
- Commercial products
- Pesticides
- Heavy metals
- Byproducts of combustion, heating and disinfection
- Solvents
The mere presence of a carcinogen in the body is not necessarily a serious health threat. EWG estimated that a small subset of the chemicals inventoried for this report (nine of the more than 400 carcinogens)* were measured at levels high enough to pose non-trivial cancer risks in most Americans – risks that generally exceed EPA safety standards. NHANES has measured only a fraction of the thousands of chemical carcinogens in our lives, but it is clear that current exposures are a real risk - not only for chemicals found at levels above government standards.
Today, scientists are looking at new ways in which chemicals likely contribute to cancer — rethinking the very notion of a chemical carcinogen. Cancer develops in stages and many carcinogens disrupt multiple or overlapping biological pathways. Scientists and physicians increasingly recognize that we need to look more expansively at the role chemicals play in cancer development. It is not enough to simply consider the effects of individual chemicals on the body. The combined effects of the many chemicals we are exposed to in real-life circumstances must also be taken into account.
The Halifax Project,1 a consortium of hundreds of scientists and physicians from around the world, recently identified the potential for chemicals that disrupt specific biological pathways, known as the hallmarks of cancer, to form carcinogenic mixtures.2 Similarly, the World Health Organization has identified 10 key mechanisms by which carcinogens act.3 These initiatives reflect the growing recognition that many carcinogens act on multiple biologic pathways that result in the cellular changes necessary for cancer development. In addition to single chemical carcinogens in isolation, scientists are learning that the disruption of multiple pathways sufficient to cause cancer can occur via the combined effect of a mixture of chemicals.
The array of carcinogens detected in humans is alarming. It underscores how much work is needed to reduce and eliminate toxic chemicals, particularly carcinogens, from our daily lives. Bans on chemicals such as PCBs and lead in gasoline have led to significant reductions of these chemicals – but government regulations can take decades to enact and politics can compromise their effectiveness.
As we fight for stronger chemical laws we should also be aware of the sources of carcinogens in our environment, food and consumers products. Reducing exposures to carcinogens, whether through regulation or personal choices, can have important health benefits.
* Acrylamide, arsenic, benzene, bromodichloromethane, bromoform, DDT, DDE, dibromochloromethane and hexachlorobenzene, discussed more fully below.
1. Measuring Carcinogens in People: Exposures come from a variety of sources
Thousands of natural and man-made chemicals are present in the environment – indoors and out, in air, food, water and consumer products. Most commercially used chemicals have never been adequately assessed for safety and most have not been biomonitored for their presence in people. Under the broken and outdated federal Toxic Substances Control Act only about 7 percent of the approximately 3,000 high volume chemicals (used in excess of a million pounds a year) have been tested for safety.
The gold standard for assessing exposure to chemical carcinogens is biomonitoring – the measurement of chemicals or their metabolites in blood, urine, breast milk, hair or other human samples.Biomonitoring is vital for accurate determination and tracking of exposures. An inventory of carcinogens measured in people would provide a knowledge base for researchers and a tool for policy-makers and regulators to assess and reduce exposures. This is especially important in light of the conclusions of the 2008-2009 report of the President’s Cancer Panel:
The Panel was particularly concerned to find that the true burden of environmentally induced cancer has been grossly underestimated. With nearly 80,000 chemicals on the market in the United States, many of which are used by millions of Americans in their daily lives and are un- or understudied and largely unregulated, exposure to potential environmental carcinogens is widespread. . . . [T]he public remains unaware of many common environmental carcinogens. . . . Most also are unaware that children are far more vulnerable to environmental toxins and radiation than adults.4
A comprehensive review by EWG of the scientific literature revealed a stunning number of carcinogens—up to 420* – that have been detected in people through biomonitoring studies. The carcinogens detected include both natural and man-made chemicals that come from a wide range of sources, including: industrial processes, commercial products, pesticides and naturally occurring materials. Table 1 provides examples of the types of carcinogens detected and their sources (the full list of carcinogens detected in people can be found in Appendices A & B).
Biomonitoring studies are a window into the amount of exposure, but do not address the source or route of exposure. Grouping the carcinogens detected in the human body into categories based on primary use can help us better understand these factors.
Table 1: Selected carcinogens measured and detected in the human body
| Chemical | Detections in NHANESa | Associated Cancer(s) | Source and Exposure | Agency & Classification |
|---|---|---|---|---|
| Industrial chemicals | ||||
| Asbestos (all forms) | not tested | Strong evidence: lung (including mesothelioma), larynx, ovary; Some evidence: pharynx, stomach, colon & rectum | Source/Use insulating material, flooring, brake pads and shoes, roofing, gaskets, cement pipes and sheets, textiles, and natural occurance. Exposure environmental: inhalation and ingestion of particles (breakdown of materials); occupational: inhalation during mining, manufacturing and repair operations. | IARC (Known); NTP (Known); EPA (Human carcinogen); CA Prop 65 |
| Benzene | 51.40% | Strong evidence: leukaemia and/or lymphoma | Source/Use component of inks, solvents, gasoline additive, and intermediate chemical (rubber, lubricants, dyes, detergents, pesticides). Exposure environmental: inhalation and some dermal absorption from industrial emissions, fuel, exhaust; occupational: inhalation/dermal exposure to solvents, paint, oil refining and working in manufacturing | IARC (Known); NTP (Known); EPA (Known/likely); CA Prop 65 |
| 1,3-Butadiene | range: >99% ; <1% (N-acetyl-S-(3,4-dihydroxybutyl)-L-cysteine ; N-acetyl-S-(1-hydroxymethyl-2-propenyl)-L-cysteine) | Strong evidence: leukaemia and/or lymphoma | Source/Use used in production of synthetic rubbers/polymers. Exposure environmental: air (mainly from point sources); occupational: petroleum refining | IARC (Known); NTP (Known); EPA (Carcinogenic); CA Prop 65 |
| Polychlorinated biphenyls (PCBs) | range: <1%->99% | Strong evidence: skin; Some evidence: breast, leukaemia and/or lymphoma, prostate, brain, liver, lung, thyroid, stomach, pancreas, colon & rectum, uterus & ovary | Source/Use electrical equipment, hydraulic machinery, fluorescent lighting fixtures, plasticizers, adhesives, flame retardants, caulk, and paints. Exposure environmental: inhalation from dust and breakdown of electrical equipment, haudraulics, and caulking; occupational: mechanical and electrical repair, construction | IARC (Known); NTP (Reasonably anticipated); EPA (Likely); CA Prop 65 |
| Chemical | Detections in NHANESa | Associated Cancer(s) | Source and Exposure | Agency & Classification |
|---|---|---|---|---|
| Consumer products | ||||
| Alcoholic beverage consumption | not tested | Strong evidence: breast, liver, colon & rectum, oral cavity, pharynx, oesophagus, nasal cavity & sinuses, larynx; Some evidence: pancreas | Source and exposure: alcohol use | IARC (Known); NTP (Known); CA Prop 65 |
| Ethylene oxide | 59.3% (N-acetyl-S-(2-hydroxyethyl)-L-cysteine) | Some evidence: breast, leukaemia and/or lymphoma | Source/Use raw material used in manufacture of chemicals for consumer goods. Exposure environmental: minor exposures through tobacco, food, skin-care products; occupational: production of ethylene oxide, use in industrial and hospital sterilization | IARC (Known); NTP (Known); CA Prop 65 |
| Perchloroethylene (Tetrachloroethylene) | 16.40% | Some evidence: leukaemia and/or lymphoma, bladder, kidney, lung, cervix, oesophagus | Source/Use dry cleaning, chemical intermediates (production of fluorocarbons), metal cleaning and degreasing. Exposure environmental: air, water, food; occupational: dry cleaning, textiles, metal industry, automotive industry, printing and cleaning | IARC (Probable); NTP (Reasonably anticipated); EPA (Likely); CA Prop 65 |
| Polybrominated Biphenyls | 87.9% (PBB-153) | Some evidence: leukamia and/or lymphoma, digestive system combined (liver, stomach, oesophagus, pancreas) | Source/Use flame retardants (primarily). Exposure air, water and soil contamination, food (milk, eggs, meat, fish) | IARC (Probable); NTP (Reasonably anticipated); CA Prop 65 |
| Tobacco(smokeless, second-hand, smoking) including: N'-Nitrosonornicotine (NNN) and 4-(N-nitrosomethylamino)-1-(3-pyridyl)-1-butanone (NNK) | 72.9%/70.4% (cotinine/NNAL) | Strong evidence: lung, oral cavity, pharynx, oesophagus, kidney, bladder, liver, stomach, colon & rectum, pancreas, nasal cavity & sinuses, larynx, uterine cervix, ovary, leukaemia and/or lymphoma; Some evidence: breast | Sources and exposure: smoking and other tobacco use | IARC (Known); NTP (Known); CA Prop 65 |
| Chemical | Detections in NHANESa | Associated Cancer(s) | Source and Exposure | Agency & Classification |
|---|---|---|---|---|
| Pesticides | ||||
| Glyphosate | not tested | Some evidence: leukaemia and/or lymphoma | Sources and exposure: mixing and application as herbicide, possible residue on foods, water and environmental contamination | IARC (Probable) |
| Permethrin | 73.4% (3-Phenoxybenzoic acid) | Some evidence: leukaemia and/or lymphoma, prostate | Sources and exposure: mixing and application as insecticide, possible residue on foods, water and environmental contamination | EPA (Likely) |
| Chemical | Detections in NHANESa | Associated Cancer(s) | Source and Exposure | Agency & Classification |
|---|---|---|---|---|
| Metals/alloys | ||||
| Arsenic and inorganic arsenic compounds | 96.20% | Strong evidence: lung, skin, bladder; Some evidence: liver, prostate, kidney | Source/Use natural occurance, pharmaceuticals, wood preservatives, agricultural chemicals, applications in mining, metallurgy, glass, and semiconductor industries. Exposure primarily contaminated food/water, some inhalation, minor occupational exposures | IARC (Known); NTP (Known); EPA (Human carcinogen); CA Prop 65 |
| Cadmium and cadmium compounds | 77.60% | Strong evidence: lung; Some evidence: prostate, kidney | Source/Use batteries, plating, stabilizers of plastics, natural occurance. Exposure environmental: ingestion of food, ambient air (minor), contaminated drinking water; occupational: inhalation during cadmium production and refining, alloy production, other smelting/plating industry | IARC (Known); NTP (Known); EPA (Probable); CA Prop 65 |
| Chromium hexavalent compounds | not tested | Strong evidence: lung; Some evidence: nasal cavity & sinuses | Source/Use pigment (textile dyes, paint, ink, plastic), corrosion inhibitor, wood preservative, metal/chrome finishing, leather tanning, given off in casting/welding, natural occurance. Exposure environmental: inhalation, contaminated drinking water; occupational: inhalation of dusts, mists, fumes and dermal contact with chromium containing products | IARC (Known); NTP (Known); EPA (Known/likely); CA Prop 65 |
| Chemical | Detections in NHANESa | Associated Cancer(s) | Source and Exposure | Agency & Classification |
|---|---|---|---|---|
| Combustion by-products/other by-products | ||||
| Bromoform | 31.90% | Evidence in animals: colon & rectum, liver | Source/Use disinfection by-product, used as fluid for mineral ore separation, lab reagent, electronics industry, formerly used as solvent for waxes, greases, oils, fire-resistent chemical. Exposure drinking water disinfected with chlorine, bromine, or bromine compounds, inhalation near factories, in laboratory use, swimming pools | EPA (Probable); CA Prop 65 |
| Polycyclic aromatic hydrocarbons (PAHs) | 98.8% (1-hydroxypyrene) | Some evidence: lung, bladder, kidney, larynx, skin, pancreas, stomach, oesophagus, prostate, leukaemia and/or lymphoma | Sources combustion of organic materials. Exposure mainly ambient air pollution, some indoor combustion sources | IARC (Known, Probable, Possible); NTP (Reasonable anticipated); CA Prop 65 |
| Chemical | Detections in NHANESa | Associated Cancer(s) | Source and Exposure | Agency & Classification |
|---|---|---|---|---|
| Solvents | ||||
| Dichloromethane (Methylene chloride) | <1.0% | Some evidence: liver, leukaemia and/or lymphoma, cervix, breast, CNS tumors, rectum, lung | Source/Use solvent. Exposure environmental: air (indoor may be higher especially from spray painting, aerosol use), contaminated soil, water (minor); occupational: industrial use | IARC (Probable); NTP (Reasonably anticipated); EPA (Likely); CA Prop 65 |
| Trichloroethylene | 1.60% | Strong evidence: kidney; Some evidence: liver, leukaemia and/or lymphoma | Source/Use solvent, degreaser, anaesthetic, heat-transfer medium, extraction agent for fats and oils, intermediate to produce chlorofluorocarbons and other chemicals. Exposure occupational: degreasing | IARC (Known); NTP (Reasonably anticipated); EPA (Carcinogenic); CA Prop 65 |
| Chemical | Detections in NHANESa | Associated Cancer(s) | Source and Exposure | Agency & Classification |
|---|---|---|---|---|
| Other | ||||
| Formaldehyde | not tested | Strong evidence: leukaemia and/or lymphoma, nasopharynx; Some evidence: nasal cavity & sinuses | Source/Use production of resins, chemical intermediate, disinfectant/preservative. Exposure environmental: natural occurance, combustion, building materials, tobacco smoke, auto exhaust | IARC (Known); NTP (Known); EPA (Probable); CA Prop 65 |
| Nitrate or nitrite (ingested) under conditions that result in endogenous nitrosation | 99.7% (nitrate) | Some evidence: stomach, bladder, kidney, colon & rectum, brain, lung, pancreas, | Source/Use natural occurance in food/water, fertilizer, food perservative. Exposure water and food | IARC (Probable) |
a Most recent available data varies for each carcinogen
Carcinogenic chemicals identified by the following authoritative agencies:
International Agency for Research on Cancer, U.S. National Toxicology Program U.S., EPA, California’s Office of Environmental Health Hazard Assessment –Proposition 65
Industrial chemicals
Industrial chemicals are used in the production of plastics, rubber and other polymers, and electrical components; in dyes, pigments, resins, solvents and adhesives; and as intermediates in the production of other industrial chemicals. Asbestos is used in insulating and fire resistant materials. Most contact with industrial chemicals comes on the job, although anyone can be exposed through contaminated air and drinking water - and to some degree from contaminated soil and food.
Cancers associated with exposure to industrial chemicals include leukemia, lymphomas, and cancers of the bladder, lung, liver, kidney, colon, rectum, pancreas, prostate and breast.
Commercial and consumer products
Around one-third of all cancers in the U.S. are caused by tobacco or alcohol. No single agent is a bigger cause of preventable cancer than tobacco - yet tobacco and alcohol are not the only commercially used chemicals associated with cancer.
Many products we routinely use contain carcinogenic chemicals, including flame retardants in furniture and other items; dry cleaning chemicals; styrene in plastics; nonstick, waterproof and grease-resistant chemicals in cookware, clothing and food wrappers; other chemicals in paints and hair coloring; and flavoring and fragrance ingredients.
Associated cancers: Tobacco and alcohol – lung and other respiratory cancers, oral cancers, breast, bladder and pancreas. Tobacco – kidney, liver, stomach and cervical cancer. Other chemicals – kidney, leukemia and/or lymphoma, liver, bladder, stomach, testis, pancreas and ovary.
Pesticides
Many pesticides have been identified as carcinogenic to some degree. People are exposed during mixing and application, pesticide drift from fields and residues on food. These exposures are not just a concern near farms. They can also occur from home use, contamination of food and drinking water, products containing wood preservatives and even some clothing.
Associated cancers: prostate, lung, liver, lymphomas and leukemias, bladder and possibly breast cancer.
Heavy Metals/Alloys
Metal molecules can bind to DNA and cause mutations. Many industrial workers come into contact with carcinogenic heavy metals and alloys, such as lead, nickel and arsenic. The public can also be exposed to trace amounts of heavy metals in food and water and even contaminated air and soil.
Associated cancers: cancers of the lung, bladder and skin and associations with liver, prostate and kidney cancers
Combustion and other by-products
Sources of combustion by-products, particularly polycyclic aromatic hydrocarbons or PAHs, include engine exhaust and air emissions from industrial facilities, power plants, and hazardous waste incinerators. Other by-products are produced when chlorine or other drinking water disinfectants react with organic solids, and when meat is cooked at high temperatures and charred.
Associated cancers: multiple cancer sites including lung, kidney, bladder, skin, stomach, prostate and non-Hodgkin lymphoma.
Solvents
Solvents are used in adhesives, in the production of pesticides and the manufacture of plastics, polymers and personal care products. Most exposures to carcinogenic solvents come in occupational settings. Exposures to the public are mostly from air contamination, especially the indoor use of paint, degreasers or some aerosols.
Associated cancers: liver, kidney and breast
* A high-end estimate. Some chemicals are measured by metabolites, or breakdown products, rather than the parent compound. Metabolites are not always specific to a single chemical and instead indicate exposure to any or all of their parent compounds. Adducts, which are the products of a chemical or its metabolite binding to DNA or protein in the body, are also sometimes measured. Our investigation did not include chemicals used primarily as medications.
2. Americans' Body Burden: Substantial exposures exist in the general population
Biomonitoring conducted as part of the NHANES surveys, although not specifically designed to track carcinogen or chemical exposures, provides a representative picture of exposures among typical Americans.
Among the carcinogens that have been measured in NHANES, some – such as arsenic, lead, nitrate, the breakdown product of DDT and the industrial chemical chloroform – were detected in nearly every person. Others that are less commonly used or encountered, such as the solvents dichloromethane and trichloroethylene and isoprene, an industrial chemical used to create polymers, were found in almost no one (Table 1, Appendices A & B).
Heavy metals and markers for many combustion by-products were among the types of carcinogens most frequently detected – found in more than 90 percent of the NHANES population. This reflects the ubiquity of these chemicals in our daily lives, resulting in repeated or continuous exposure.
Pesticides and their metabolites were detected less frequently, in one-third to two-thirds of those surveyed. Exposure to pesticides is intermittent, and many stay in the body for only a short period of time. Consequently, pesticides are less likely to be detected in NHANES than a study that targets biomonitoring sampling around the time of application, which is a more accurate assessment of exposure.
On the opposite end of the spectrum are PCBs and other chemicals that persist in the environment and our bodies for long periods of time. PCBs were banned in the U.S. in 1979, but they were still detected in between 5 percent to 100 percent of the NHANES population, depending on the specific PCB (there are 209 different PCB congeners.) Although levels have gone down since the ban, people are still exposed to PCBs as older products made with these chemicals, such as electrical equipment, hydraulics, and caulking begin to break down. Researchers at Harvard University have found PCBs released from old caulking in public buildings, including schools.5
The body burden has also declined for other chemicals that have been banned or phased out:
- The pesticide DDT, banned in the U.S. in 1972.
- Lead, phased out of gasoline starting in 1975 and completely banned in 1995.
- The Teflon chemical PFOA, for which phase-out was complete in 2015, but still detected in 99 percent of the NHANES population.
Certain populations, particularly workers in occupational settings, can have exposures to chemical carcinogens that are not generally encountered by the general public. The solvents and several of the industrial chemicals, among others, listed in this report (Appendix A) are almost entirely occupational concerns. They are primarily used in production processes and are not present in materials that would exposure the general population. (The exception is industrial pollution contaminating the environment).
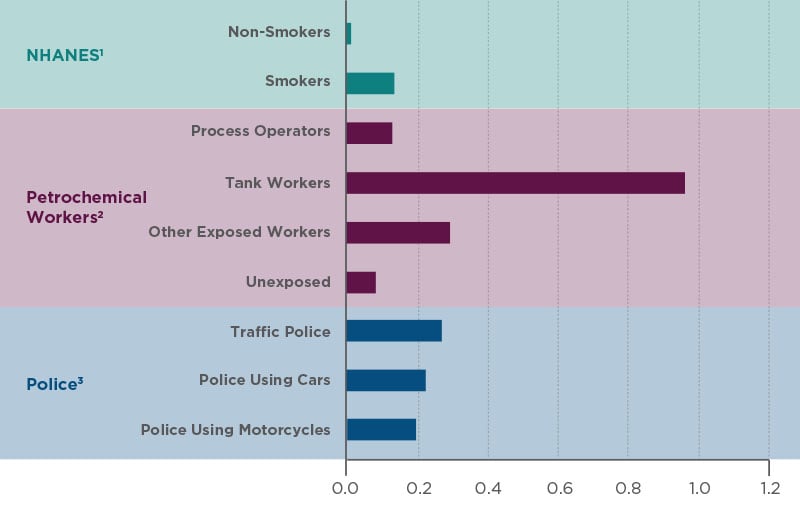
In addition, occupational exposures can be magnitudes of order higher than levels experienced by the general public. Average* concentrations of benzene, which is a component of petroleum and found in tobacco smoke, in the blood of workers maintaining crude oil tanks were more than seven times higher than even the typical smoker in the U.S. (Figure 1).6 Police officers exposed to traffic pollution in Rome had benzene levels about twice as high as smokers in the U.S.7 Industrial processes can also pollute the environment, resulting in high exposures to the surrounding area. After the Deep Water Horizon oil spill disaster in the Gulf of Mexico, nearby residents had blood benzene levels that were about five times that of the typical non-smoker.8 It is no surprise that detrimental health effects are often first experienced and detected in highly exposed occupational settings.
* Geometric mean is similar to the more familiar arithmetic mean. An arithmetic mean is an average of added numbers, whereas a geometric mean is an average of multiplied numbers—making it less influenced by extreme values. Among groups of people, most usually have exposures to chemicals at low to moderate levels and a few have very high levels. A geometric mean, therefore, is a more robust description of the average level.
3. Cancer Risk: The contribution of chemicals to the cancer burden
The presence of a chemical in our body is not necessarily harmful9 - risk depends on the amount of exposure and the inherent toxicity of the chemical. These factors are the starting points for determining the dose-response relationship – how much exposure to a chemical is needed to increase our risk of disease by 10 percent, 50 percent or more. Estimating these risks can be extremely difficult when the only information available is the concentration of a chemical measured by biomonitoring.
One potential solution is the use of biomonitoring equivalents, or BEs – – tools that translate measured chemical concentrations to health risks, usually based on government safety standards.10 For cancer, a BE estimates the measured concentration of a chemical that would on average result in a one-in-a-million to 1-in-10,000 chance of getting cancer, the usual standards used in EPA risk assessments.
How much risk do carcinogens in the body pose to Americans? We can get a glimpse by applying BEs, which were available for nine carcinogens in this report, to exposure levels in the NHANES surveys (Figure 2).
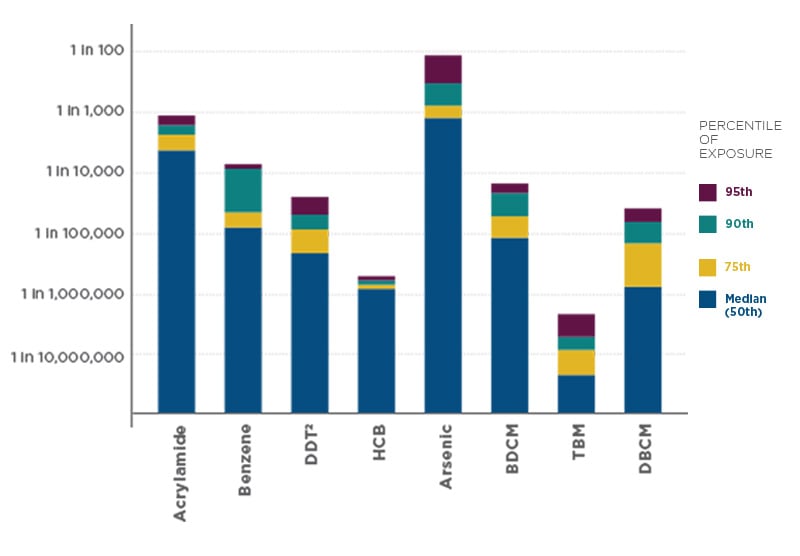
Chemical carcinogens with available BE information:
- acrylamide, used in the production of industrial polymers and produced when starchy foods are cooked at high temperatures
- arsenic, a naturally occurring metal
- benzene, a component of petroleum
- bromodichloromethane, bromoform and dibromochloromethane, by-products produced when chlorine, used to disinfect water, reacts with organic matter
- DDT & DDE, pesticide (banned in the U.S.) and its breakdown product
- hexachlorobenzene, a fungicide and industrial chemical, also a by-product in the production of chlorinated solvents
We used BEs to approximate the proportion of the U.S. population that may be exposed to certain chemicals at levels that exceed what EPA considers to be an acceptable risk.11
- More than half of the NHANES population had levels of arsenic and acrylamide that were estimated to exceed a 1-in-10,000 cancer risk. More than 10 percent had levels of benzene that exceeded that degree of risk.
- The majority of Americans tested also had levels of DDT and DDE,* benzene, hexachlorobenzene, bromodichlorobenzene and dibromochloromethane that exceeded the one-in-a-million risk threshold.
- Only for bromoform were estimated cancer risks for the general population less than one in a million.
Concentrations of these carcinogens did not vary greatly between older and younger people, indicating that exposures and risk for these chemicals start accruing early.
Although biomonitoring equivalents are useful they should be interpreted with caution.
They assume a measured biomarker concentration represents a person's average lifetime exposure of an individual. This may be a reasonable assumption for chemicals that are persistent or chemicals to which we are continuously exposed, but not for chemicals that quickly move through the body, are easily metabolized or have intermittent exposures. Those require repeated samples over time to tell the story of a person’s lifetime exposure. Risk is also highly dependent on genetics and individual differences in metabolism. Finally, BE data was available for only a few select chemicals that may not be representative of risks for other carcinogens.
What the estimates do provide is an indication that at least a small subset of the hundreds of carcinogens measured in humans are contributing to non-trivial increases in cancer risk. These risks may be even greater when we consider that the estimates are only for individual chemicals and do not account for how combined exposures to multiple chemicals may increase risk.
* DDT exposure is customarily calculated from the sum of the levels of DDT and its breakdown product DDE.
4. The Hallmarks of Cancer: Expanding how we search for carcinogens
How combinations of chemicals interact in our bodies is not well understood. We are repeatedly exposed to tobacco, alcohol, heavy metals and combustion by-products, which target many of the same body tissues and organs - and when combined may have the potential to dramatically increase the risk cancers.
Now scientists are rethinking how chemicals may contribute to cancer. New research from the Halifax Project suggests that mixtures of chemicals – even ones not known to be carcinogenic on their own – could cause cancer by disrupting multiple mechanisms known as the hallmarks of cancer.1,2
The hallmarks listed below are the characteristics that distinguish cancer cells – abnormal cells gone rogue, dividing and growing beyond the control of our body – from normal cells.12,13
The Hallmarks of Cancer Cells
Self-sufficient cell division—cancer cells grow and divide on their own
Insensitive to signals to stop cell division—cancer cells do not stop growing and dividing when signaled by the body
Resist cell death—cancer cell do avoid normal programmed cell death that removes old or damaged cells from the body
Limitless reproductive potential—cancer cells can replicate many more times than normal cells
Create own blood supply—cancer cells can stimulate the formation of blood vessels
Ability to invade other organs (metastasize)—cancer cells can spread from one organ to another
Ability to survive with little oxygen—cancer cells can switch to anaerobic respiration when oxygen supplies are low
Evade the immune system—cancer cells can avoid destruction by our body’s immune system
Genomic instability—cancer cell DNA is susceptible to changes in genes and gene expression
Inflammation—inflammation can promote conditions that can damage DNA
The scientists of the Halifax Project identified 85 chemicals common in the environment that are capable of disrupting hallmark pathways in the body – and the search for these types of chemicals is just beginning. What is alarming is these chemicals are not only common in the environment, they are common in people as well.
In NHANES, 34 of these hallmark-disrupting chemicals or their metabolites have been measured and detected in Americans' bodies. (Appendix C) That is significant because it means these chemicals are pervasive among the general population. Even if exposures to these chemicals do not occur simultaneously in the environment, many could still be circulating in the body at once.
The hypothesis of the Halifax Project – discussed in EWG’s Rethinking Carcinogens report1 – is that the same biological mechanisms by which many known carcinogens cause cancer can also be achieved through the combined effects of multiple chemicals.
Take the most well known carcinogen, tobacco, itself a mixture of chemicals including other known carcinogens NNN and NNK.14 Tobacco causes cancer through a multitude of hallmarks (in italics) and other biological mechanisms:
- It causes mutations in the genes regulating cell growth, that suppress tumors and other genes that result in uncontrolled cell proliferation and genomic instability.
- It affects receptors on cells causing resistance to cell death, increased ability for a cell to create its own blood supply and increased cellular transformations.
- It also causes oxidative damage—free radicals that can react with and damage DNA, inflammation and DNA methylation, a chemical process that can modify how genes function.
Mechanisms of carcinogenesis for other known carcinogens similarly involve hallmark processes. Based on these mechanisms, it is a good bet that mixtures of hallmark-disrupting chemicals could have combined effects equivalent to individual carcinogens.
Here is how a mixture of chemicals we are commonly exposed to can disrupt a similar series of pathways as tobacco:
- Bisphenol A (BPA), found in many plastics that store food and beverages, can disrupt cell proliferation and result in resistance to cell death and inflammation.
- Heavy metals, which we can be exposed to through drinking water, some seafood and or occupational exposures, can cause genomic instability.
- PFOS, a chemical used as a stain repellant on fabrics, can increase a cell’s ability to create its own blood supply.
That does not mean those combination of chemicals are as toxic as tobacco. They are nowhere near as powerful disrupters of those hallmark pathways, and there are many other factors involved in tobacco’s toxicity. There is no evidence yet of that particular combination of chemicals even being carcinogenic. It is merely an example of how the series of events that lead single chemicals to cause cancer could occur through exposure to mixtures of chemicals.
The potential for chemical mixtures of chemicals to cause cancer is supported by an investigation by the International Agency for Research on Cancer, part of the United Nations World Health Organization. IARC identified 10 key characteristics of mechanisms by which known carcinogens act.3 These characteristics, many of which are hallmark pathways, recognize that cancer develops in multiple stages. Many carcinogens act on multiple pathways and cause a series of biological changes in cells.
This line of thinking sets the stage for broader consideration of how chemicals contribute to cancer, rather than narrowly focusing on isolated chemicals or mechanisms. To evaluate this idea will require toxicity testing and regulatory standards that reflect the true nature of human exposure by considering the combined effects of chemicals on the body.
5. Conclusion And Recommendations: Reducing risks from chemical exposures
It is clear, we are exposed to and take into our bodies an incredible number of chemicals that are known or possible carcinogens. Biomonitoring data shows that exposures to a many cancer-causing chemicals are not limited to special populations such as industrial workers but are present in everyday life.
Biomonitoring studies are incredibly valuable for accurately measuring and tracking human exposure to chemicals. This inventory of carcinogens is important for research aimed at uncovering the links between chemicals and disease and also for policy makers to understand the risks that exist among people. In fact, scientists at the reputable Silent Spring Institute in Massachusetts conducted a full study to identify potential biomarkers that may cause breast cancer for those very reasons.15
Detection of carcinogens in the human body is only part of the story. Thanks in large part to anti-smoking smoking campaigns, the incidence of lung cancer and some other cancers have begun to decline or level off. But 45 years after passage of the National
Cancer Act, we have not seen the declines hoped for.
Rates of liver, kidney and many childhood cancers continue to rise. Based not only on detections, but measured concentrations, at least a portion of the chemical carcinogens found in the majority of Americans are likely contributing to meaningful increases in cancer risk.
Genetics and bad luck play a big part in who gets cancer but chemical exposures also play a major role. The ubiquity of chemicals in modern life means we cannot eliminate exposure, but we have some control through our consumer choices, along with factors such as diet and exercise. The 2010 Surgeon General’s report on tobacco concluded that quitting smoking at any age can drastically reduce a smoker’s risk of cancer – by up to 50 percent in just five to 10 years.16 The risks from most other chemical carcinogens are very small in comparison, but it is an important reminder that reducing exposures can have real health benefits.
Scientists are rethinking how chemicals contribute to cancer, recognizing that chemicals can cause cancer through overlapping biological pathways. Advancing this idea will require a far more robust appraisal for how we determine toxicity and much tougher chemical regulations.
Federal law fails to provide the EPA and FDA with the tools needed to ban or even limit carcinogens in everyday products. Regulations on chemicals in cleaners, cosmetics, food and other consumer products should all be strengthened to require expedited review of the most dangerous substances, to ensure they meet the tough “reasonable certainty of no harm” standard, to provide extra protection for vulnerable populations like children, and to ensure that that EPA and FDA have enough data and resources to do the job.
Federal law should also preserve a role for state regulators, who have served as the only cop on the chemical beat for decades, and should not permit industry-financed “safe lists” of substances that get a free pass from regulation. Consumers should have the right to know the chemicals used in their products, including chemicals used in fragrance and flavors.
More research is also needed investigating the role of chemical exposures and the environment on the development of cancer. In his final State of the Union speech, President Obama announced the creation of a National Cancer Moonshot Initiative to find a cure for cancer in our lifetime. The goal is to break down barriers stifling scientific research, foster scientific collaborations and fund promising and novel research.
But the focus is on funding to advance treatment and research in genetics and molecular biology, largely ignoring environmental causes of the disease and prevention. Almost all of the scientists selected for the Blue Ribbon Panel to advise the initiative are entirely clinically focused.
Improved treatments and better understanding of the genetics and molecular biology of cancer are crucial in the battle to defeat this disease. But, as the findings of this report make clear, our environment plays a critical role as well.
Advances in treatment have improved survival by nearly 20 percent in the last 20 years. More promising treatments, such as immunotherapies, are on the horizon. But cancer is hundreds of diseases, not one, each with distinct etiologies. We are not searching for a single cure. Moreover, the costs of developing cancer, even if successfully treated, can be staggering. In addition to the tremendous physical and emotional toll, cancer treatments can result in a substantial financial burden. Financial stress, including increased rates of bankruptcy, can lead to poor survival and other adverse health outcomes among cancer patients.17
The only concrete agenda related to prevention outlined in President Obama’s Moonshot Initiative is for screening and vaccination. Understanding the environmental causes of cancer are also necessary to prevent and defeat this disease. The World Health Organization estimates that as much as 19 percent of cancers are due to environmental exposures.18 We have seen the success of smoking cessation efforts—reducing the rate of lung cancer by more than 25 percent in the last 25 years.
The incredible number of human carcinogens detected in this report demonstrates the burden of environment on human health. It is imperative the Moonshot include federal funding for the investigation of the environmental causes of cancer and the development of prevention initiatives in that arena.